While no one wants to dwell too much on dying, making arrangements for that inevitable event is very important.
Dr Tony Holohan, former Chief Medical Officer, and now an Irish Hospice Foundation (IHF) board member, believes that the updated Think Ahead Planning Pack, available free from the IHF, is a great tool to help you get your wishes down on paper.
Say, for instance, that you become very ill or are injured, would you want to be placed on a ventilator (a mechanical breathing machine)? Would you want to be artificially fed? Would you like your organs to be donated if you died in an accident?
Ease stress on family members
Filling out the three-section planning pack will mean that your wishes related to all this and more will be recorded, easing stress for family members at a distressing and emotional time.
“Conversations about illness, dying and death should happen in every home in Ireland before there is a crisis,” he says.
“If you don’t think about all these things ahead of time, it makes it more difficult for everyone around you, so having those conversations well ahead of time is important.”
The advice when recording your preferences and choices for your future care through illness, end of life and after death is to think about what you want, talk to someone about your wishes and tell them where the form is.
Dr Holohan used the planning pack when his late wife was ill, he says.
“We talked about what we wanted and filling in the information was a way of structuring our conversation. It’s not a single conversation, you fill it out over a period of time, but the important thing is to complete it.”
Dr Tony Holohan at the launch of the updated Think Ahead Planning Pack
He is delighted to be associated with such an important IHF initiative, he says, and he therefore advocates getting the pack and not putting off the task of filling it in.
“You’ll have the comfort of knowing that if something does happen to you [where you can’t speak for yourself] your family members will be able to carry out your wishes instead of saying, ‘God, I wonder what he/she would have wanted’. It means there is no ambiguity for families and loved ones, our wishes are met and there is great comfort in that for all involved.”
What’s involved
The Think Ahead Planning Pack is divided into three sections:
1 My personal wishes and care plan
This is a booklet where you fill in:
Your health history, doctor’s names, blood group etc, medical conditions and allergies, if any.Where you would like to be cared for if very ill eg transferred to hospital or not. Your personal wishes, eg I want religious items around me or not, photos of pets etc and what you like doing, eg reading the newspaper/watching sport. Your legal arrangements – solicitor’s name, where your will is stored, details of enduring power of attorney.Your financial records – bank accounts (don’t record PINs or online codes), credit cards, insurance details, pensions and State pension numbers, mortgage details, loans, assets (name of accountant or stockbroker if any). Location of important documents. Also include a list of what you want to remain unread/disposed of after your death, eg personal journals.Your digital legacy – following a death, technology companies can either delete accounts or change your social media page to a memorialised account at the request of a close family member or the person who has an enduring power of attorney. List your accounts (eg, Facebook and WhatsApp) and say whether to delete or memorialise.After death and funeral arrangements – type of ceremony, final resting place, organ donations, a list of people you would like informed of your death.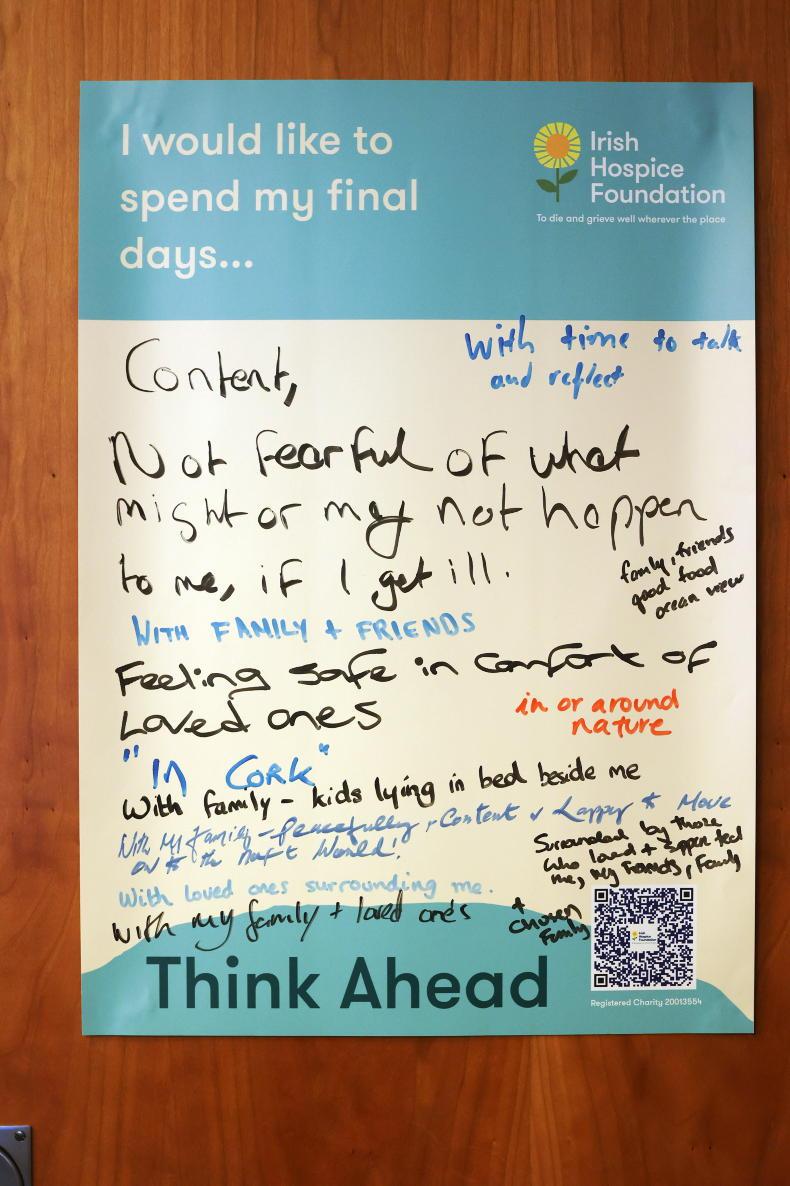
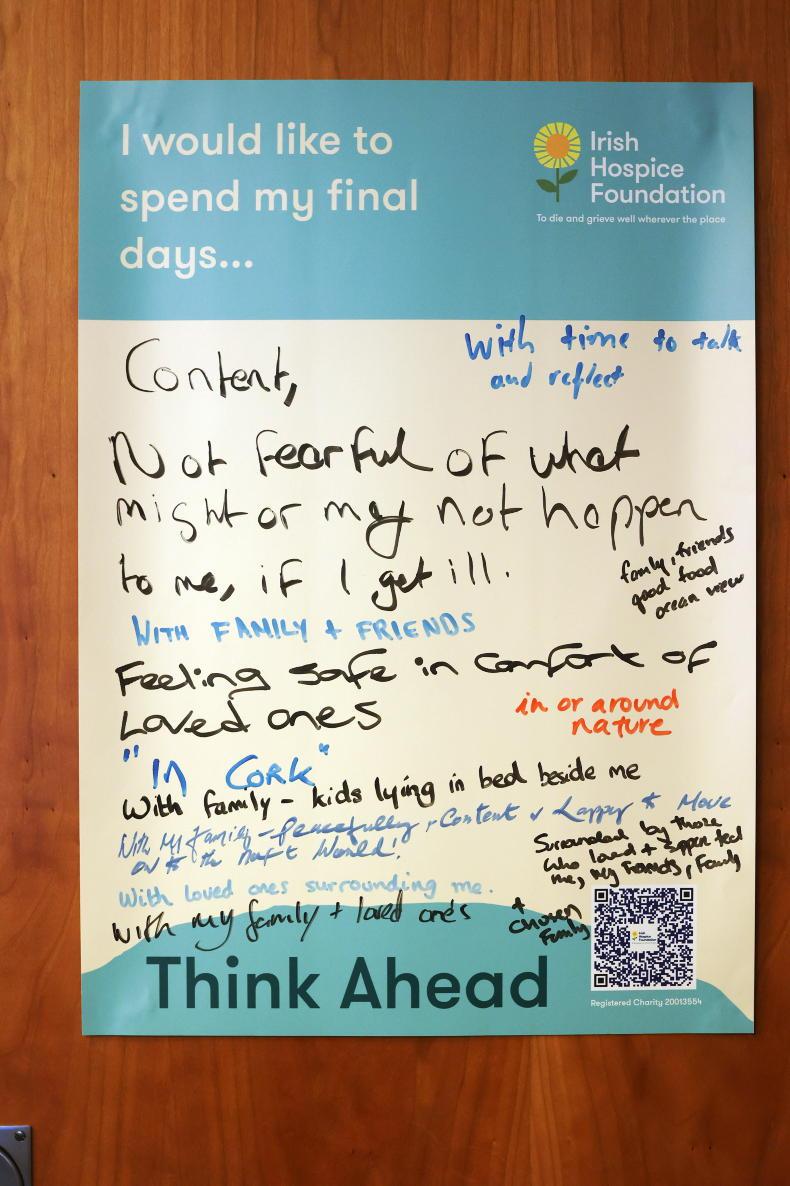
An example of someone's thoughts about end of life care
Store this copy securely and let those who are important to you know where it is. Update regularly.
2 My advance healthcare directive
This is where you record your healthcare choices and appoint somebody to speak on your behalf should you lack decision-making capacity to advocate for yourself through illness, accident or mental distress. This document is legally binding when properly signed and witnessed and should be reviewed regularly as your decisions may change over time. It lists:
Healthcare treatments I refuse, eg artificial feeding.Healthcare treatments I request, eg I wish to be treated at home if possible.The person I appoint to speak on my behalf (my designated healthcare representative).Signing and having this document witnessed by two people makes it legally binding. Two witnesses are required, one family member, one not, to avoid the risk of coercion.
3 My medical summary form
This is a summary of your care and treatment decisions and preferences, to be shared with your GP/specialist.
Ahead of time
There isn’t a specific age to fill the form in at, according to Dr Holohan. Rather, the key thing is to do it well ahead of time.
“The reality is that as we get older, we think more about things like wills,” he says.
“We all know we are going to die at some point and that wills should be written if we have family or property. Making a will or filling out the Think Ahead Planning Pack is not going to make illness or death progress any faster, but if something does happen, it makes it easier for family members who have to deal with your affairs and wishes. We’d all want to do that for those we love. It’s not just about making things easier for yourself.”
Starting the conversation
He suggests choosing the person you start the end-of-life conversation with carefully.
“It might be a trusted friend, a family member, maybe not your spouse who is going to be immediately upset at the prospect of such a conversation. Allow yourself to get used to articulating these ideas, then prepare yourself for introducing that conversation with someone you trust.”
The Irish Hospice Foundation has some guidance about how to start such a conversation in its conversations over a cuppa series.
Vol.1: Dying to talk – how to have a general conversation.Vol.2: When someone you know is seriously ill – what to say when you don’t know what to say.Vol.3: When someone you love is seriously ill.Vol.4: When you are seriously ill. See www.thinkahead.ie or https://hospicefoundation.ie/i-need-help/i-want-to-think-ahead-old/start-to-talk/
Should be normal in hospital
Dr Holohan is in favour of having this planning pack distributed to hospital or nursing home and GP patients routinely. “The more we can normalise this the better,” he says. “Patients should know that it is a routine part of what those services are going to ask about and not a case of ‘oh, gosh they must think I’m about to die’. These conversations shouldn’t wait until someone is in intensive care or about to be admitted to a hospice. There is pressure on and urgency then trying to clarify what someone’s wishes regarding treatment are. Thinking all these things out beforehand makes everything easier.”
Legally binding
Following the passing of legislation in 2022, the advance care directive, signed and witnessed, is now legally binding.
“This will give protection to your wishes and allow you to have a designated healthcare representative who can say what you want and don’t want in terms of treatment,” he adds.
“The evidence is that when people think about these things, they tend not to choose what isn’t going to add quality and quantity to their life.”
Dr Holohan, whose grandparents were farmers, advises everyone to use the Think Ahead Planning Pack.
“Sometimes life gets in the way and something that isn’t immediately urgent gets put on the shelf, but filling this out is important the same as updating wills, so my basic message, including to farmers, is not to put it off.”
The Irish Hospice
Foundation says:
Many people don’t die as they might have wished to, or in the place that they wanted to be. They may not have left a will, expressed their wishes about their funeral or said what they wanted to say to those closest to them. These can be difficult and emotional subjects to deal with, but it’s in everybody’s interest to be able to:Share your wishes while there is still time.Consider updating your document once a year. Put a reminder on your phone or calendar to review it on a date that is important to you.Store your copy securely, as you would a will.Survey
The Irish Hospice Foundation carried out a survey in 2022, which identified that after the pandemic of the last couple of years, 47% of people were giving more thought to their own end-of-life wishes and 56% have talked to their friends and family about death and dying. For more information, see
www.thinkahead.ie
Read more
Health: autism dog making a big difference to a Leitrim family
Closure crisis in nursing home sector
While no one wants to dwell too much on dying, making arrangements for that inevitable event is very important.
Dr Tony Holohan, former Chief Medical Officer, and now an Irish Hospice Foundation (IHF) board member, believes that the updated Think Ahead Planning Pack, available free from the IHF, is a great tool to help you get your wishes down on paper.
Say, for instance, that you become very ill or are injured, would you want to be placed on a ventilator (a mechanical breathing machine)? Would you want to be artificially fed? Would you like your organs to be donated if you died in an accident?
Ease stress on family members
Filling out the three-section planning pack will mean that your wishes related to all this and more will be recorded, easing stress for family members at a distressing and emotional time.
“Conversations about illness, dying and death should happen in every home in Ireland before there is a crisis,” he says.
“If you don’t think about all these things ahead of time, it makes it more difficult for everyone around you, so having those conversations well ahead of time is important.”
The advice when recording your preferences and choices for your future care through illness, end of life and after death is to think about what you want, talk to someone about your wishes and tell them where the form is.
Dr Holohan used the planning pack when his late wife was ill, he says.
“We talked about what we wanted and filling in the information was a way of structuring our conversation. It’s not a single conversation, you fill it out over a period of time, but the important thing is to complete it.”
Dr Tony Holohan at the launch of the updated Think Ahead Planning Pack
He is delighted to be associated with such an important IHF initiative, he says, and he therefore advocates getting the pack and not putting off the task of filling it in.
“You’ll have the comfort of knowing that if something does happen to you [where you can’t speak for yourself] your family members will be able to carry out your wishes instead of saying, ‘God, I wonder what he/she would have wanted’. It means there is no ambiguity for families and loved ones, our wishes are met and there is great comfort in that for all involved.”
What’s involved
The Think Ahead Planning Pack is divided into three sections:
1 My personal wishes and care plan
This is a booklet where you fill in:
Your health history, doctor’s names, blood group etc, medical conditions and allergies, if any.Where you would like to be cared for if very ill eg transferred to hospital or not. Your personal wishes, eg I want religious items around me or not, photos of pets etc and what you like doing, eg reading the newspaper/watching sport. Your legal arrangements – solicitor’s name, where your will is stored, details of enduring power of attorney.Your financial records – bank accounts (don’t record PINs or online codes), credit cards, insurance details, pensions and State pension numbers, mortgage details, loans, assets (name of accountant or stockbroker if any). Location of important documents. Also include a list of what you want to remain unread/disposed of after your death, eg personal journals.Your digital legacy – following a death, technology companies can either delete accounts or change your social media page to a memorialised account at the request of a close family member or the person who has an enduring power of attorney. List your accounts (eg, Facebook and WhatsApp) and say whether to delete or memorialise.After death and funeral arrangements – type of ceremony, final resting place, organ donations, a list of people you would like informed of your death.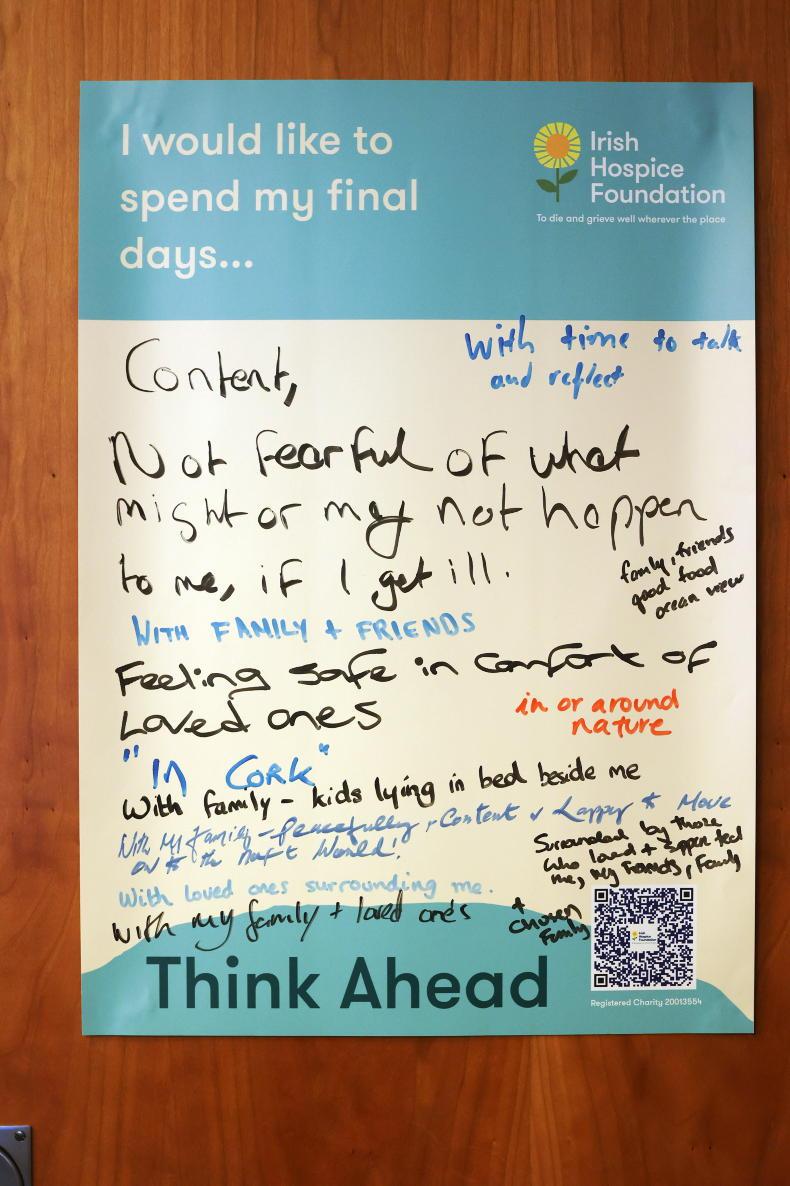
An example of someone's thoughts about end of life care
Store this copy securely and let those who are important to you know where it is. Update regularly.
2 My advance healthcare directive
This is where you record your healthcare choices and appoint somebody to speak on your behalf should you lack decision-making capacity to advocate for yourself through illness, accident or mental distress. This document is legally binding when properly signed and witnessed and should be reviewed regularly as your decisions may change over time. It lists:
Healthcare treatments I refuse, eg artificial feeding.Healthcare treatments I request, eg I wish to be treated at home if possible.The person I appoint to speak on my behalf (my designated healthcare representative).Signing and having this document witnessed by two people makes it legally binding. Two witnesses are required, one family member, one not, to avoid the risk of coercion.
3 My medical summary form
This is a summary of your care and treatment decisions and preferences, to be shared with your GP/specialist.
Ahead of time
There isn’t a specific age to fill the form in at, according to Dr Holohan. Rather, the key thing is to do it well ahead of time.
“The reality is that as we get older, we think more about things like wills,” he says.
“We all know we are going to die at some point and that wills should be written if we have family or property. Making a will or filling out the Think Ahead Planning Pack is not going to make illness or death progress any faster, but if something does happen, it makes it easier for family members who have to deal with your affairs and wishes. We’d all want to do that for those we love. It’s not just about making things easier for yourself.”
Starting the conversation
He suggests choosing the person you start the end-of-life conversation with carefully.
“It might be a trusted friend, a family member, maybe not your spouse who is going to be immediately upset at the prospect of such a conversation. Allow yourself to get used to articulating these ideas, then prepare yourself for introducing that conversation with someone you trust.”
The Irish Hospice Foundation has some guidance about how to start such a conversation in its conversations over a cuppa series.
Vol.1: Dying to talk – how to have a general conversation.Vol.2: When someone you know is seriously ill – what to say when you don’t know what to say.Vol.3: When someone you love is seriously ill.Vol.4: When you are seriously ill. See www.thinkahead.ie or https://hospicefoundation.ie/i-need-help/i-want-to-think-ahead-old/start-to-talk/
Should be normal in hospital
Dr Holohan is in favour of having this planning pack distributed to hospital or nursing home and GP patients routinely. “The more we can normalise this the better,” he says. “Patients should know that it is a routine part of what those services are going to ask about and not a case of ‘oh, gosh they must think I’m about to die’. These conversations shouldn’t wait until someone is in intensive care or about to be admitted to a hospice. There is pressure on and urgency then trying to clarify what someone’s wishes regarding treatment are. Thinking all these things out beforehand makes everything easier.”
Legally binding
Following the passing of legislation in 2022, the advance care directive, signed and witnessed, is now legally binding.
“This will give protection to your wishes and allow you to have a designated healthcare representative who can say what you want and don’t want in terms of treatment,” he adds.
“The evidence is that when people think about these things, they tend not to choose what isn’t going to add quality and quantity to their life.”
Dr Holohan, whose grandparents were farmers, advises everyone to use the Think Ahead Planning Pack.
“Sometimes life gets in the way and something that isn’t immediately urgent gets put on the shelf, but filling this out is important the same as updating wills, so my basic message, including to farmers, is not to put it off.”
The Irish Hospice
Foundation says:
Many people don’t die as they might have wished to, or in the place that they wanted to be. They may not have left a will, expressed their wishes about their funeral or said what they wanted to say to those closest to them. These can be difficult and emotional subjects to deal with, but it’s in everybody’s interest to be able to:Share your wishes while there is still time.Consider updating your document once a year. Put a reminder on your phone or calendar to review it on a date that is important to you.Store your copy securely, as you would a will.Survey
The Irish Hospice Foundation carried out a survey in 2022, which identified that after the pandemic of the last couple of years, 47% of people were giving more thought to their own end-of-life wishes and 56% have talked to their friends and family about death and dying. For more information, see
www.thinkahead.ie
Read more
Health: autism dog making a big difference to a Leitrim family
Closure crisis in nursing home sector









SHARING OPTIONS