Every year in Ireland, approximately 350 people are diagnosed with multiple myeloma – a cancer of the plasma cells that are made in the bone marrow. Although it is a rare and incurable blood disorder, it is treatable and some patients can live a normal life.
To further explain, multiple myeloma is an abnormal protein produced in multiple sites (bones) in the body, causing bone damage and pain. Kidney damage also occurs because calcium is leaked from the damaged bones.
The most common symptoms, therefore, are persistent bone or back pain, as well as kidney problems, anaemia, recurring infections and fatigue.
However, the news related to this type of cancer is very positive, according to Mary Kelly, registered advanced nurse practitioner in haematology, based at the Midlands Regional Hospital, Tullamore. She has cared for myeloma patients for 25 years and is in no doubt about the progress in treatments.
“Patients with multiple myeloma are now living much longer as a result of the great treatments available,” she says. “Five-year patient survival rates have increased from 24% to over 70% so it’s very good news.”
Concern about patients back in 2006 led Mary to write a thesis on the lived experience of multiple myeloma patients. She found that isolation, lack of support and general lack of awareness of the illness were major concerns.
She subsequently set up the support charity, Multiple Myeloma Ireland in 2008, which is based in the Dóchas Centre in Tullamore. It is the first and longest-running support and information group for people living with the disease.
Groups across the country have now sprung up as a result and a podcast began during lockdown called Living with Myleoma which has been nominated for a Bullseye award in the Irish Podcast Awards.
Mary has three key messages for anyone who is newly diagnosed.

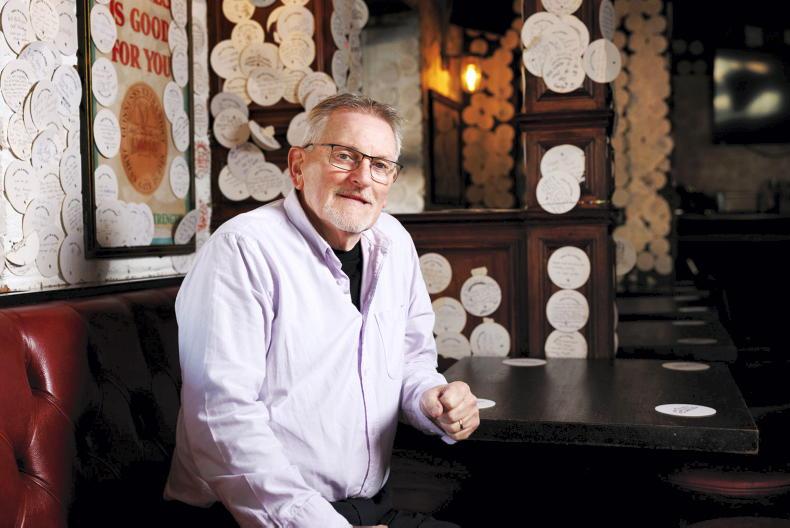
Advanced nurse practitioner in haematology Mary Kelly pictured with Mag.
“Firstly, this is a very treatable condition. Secondly, anyone with symptoms should get them checked out quickly and thirdly, there is a lot of support for anyone with this illness,” she says.
However, making a diagnosis can be challenging. “A lot of tests are needed and that’s one of the challenges for healthcare professionals in the community. GPs may only see one case during their career so they are not looking for it. It can often be a combination of vague symptoms; who isn’t tired, who doesn’t have back pain, or some bone pain? However, persistent, severe pain are indicators.
“Multiple myeloma can sometimes be missed, so if you’ve got recurring symptoms you should be advocating with your GP for further investigation.”
Mag Kirwan’s story
Mag and her husband, Ger, run Goatsbridge Trout Farm near Thomastown, Co Kilkenny. The 59-year-old developed a love of fitness training in 2015, but in late 2019 she got a bad pain in her shoulder.
“I went to my local physio first and then to a second physio as it wasn’t getting better,” explains Mag.
“Anti-inflammatories were suggested so I had to contact my GP to get a prescription. As it happened, a new doctor looked at blood tests that I had done a few months earlier. Noticing some unusual levels, he advised getting more tests done. After an MRI, he rang to say I had a mass (a tumour) in my shoulder.”
A bone specialist then diagnosed early multiple myeloma but after a bone biopsy and a PET scan, Mag was told that it was full-blown multiple myeloma.
“This meant a change in my treatment plan, eight months of chemotherapy and the harvesting of my own stem cells in order for me to develop new bone marrow.”
Mum-of-four Mag found her eldest son, Ned’s 21st birthday in February 2020 particularly difficult. “I kept wondering if I’d be around to see the next one turn 21, and so on,” she says.
If you’re lucky and you keep your body and head right, you can live long and well with this. That’s what I believe
However, once she had her treatment plan, she felt more positive. “I knew it would take a year or two of consolidation treatment after the stem cell transplant. During that time I worked when I could and isolated when I had to.”
Nearly three years on, Mag says practising gratitude helps her get on with life.
“I have a lot going for me. Fifteen years ago there were one or two drugs available – now several new ones have been approved so, even though it’s not curable, it’s treatable.
“If you’re lucky and you keep your body and head right, you can live long and well with this. That’s what I believe. I don’t think too far ahead, I trust my consultant and my trainer. I have a great family and I feel really blessed.”
Mag, one of 10 from the Goresbridge Horse Sales family, believes that she has learned resilience over her lifetime.
“My mother was 42 and two months away from having her 10th child when my father died. My brother Jack died later, aged 10, of measles. My mother continued to grow the family business to international success and reared and educated us all.
“Life teaches you resilience so then when something like this happens you’re able to fight it and get on with it. I really believe that the power of the mind is incredible and that exercise is great medicine.”
Dermot O’Leary’s story
When dad-of-five Dermot, a 65-year-old dairy farmer from Bandon, Co Cork, had a routine blood test in September 2015, it showed high protein levels in his blood. At first prostate issues were suspected but a few months later, in January 2016, multiple myeloma was diagnosed.
“I had no symptoms,” he says, “but looking back I’d often fall asleep at the table after supper. Maybe that was the start of it and I just didn’t recognise it.
“I was glad to have a diagnosis in a way but my doctor said ‘you do realise this is cancer?’ I didn’t I suppose, but it sank in over a couple of days.”
Dermot attended a support meeting in Tullamore in March 2016, ahead of starting treatment in April.
“I had a good chat with the people there,” he says, “and felt, after that, that I could handle what was happening. I was calving cows at the time and working away as normal. I wouldn’t be a worrier. I just got on with it.”
Looking back I’d often fall asleep at the table after supper. Maybe that was the start of it and I just didn’t recognise
He underwent a stem cell transplant, which involves tests to assess your general level of health, harvesting to collect the stem cells to be used in the transplant, conditioning ie treatment with chemotherapy and/or radiotherapy to prepare your body for the transplant. Then there is the transplantation of the stem cells and, after that, recovery.
“They take out stem cells (enough for two treatments if needed),” Dermot says, “then put them back in again following chemotherapy. There were a few tough days, but it wasn’t the end of the world either,” he says.
He has been on a maintenance drug called Revlimid since then and an aspirin every morning to avoid clots.
Dermot has been on the board of Multiple Myeloma Ireland since 2019 and set up a support group in Cork.
“Early diagnosis is vital,” he insists. “There are horror stories where sports people who have pain in their back just assume it’s the legacy of sport. The sooner you get myeloma diagnosed, the better. That’s why we’re trying to get the word out.
“Our support groups meet every second month. Being a member helps you feel that you’re not alone and you learn from others too.”
Multiple myeloma is a blood cancer that develops in plasma cells in the bone marrow – the soft, spongy tissue at the centre of your bones.
Myeloma affects multiple places in the body where bone marrow is normally active in an adult, ie within the bones.
Stem cell transplants for multiple myeloma sees a person’s own stem cells removed from the bone marrow and stored until needed. The cells given in a transplant can grow into healthy blood cells in the bone marrow.
Multiple Myeloma Ireland is now lobbying for funding for a database of patients living with the illness.
For more information, email info@multiplemyelomaireland.org or see multiplemyelomaireland.org or cancer.ie
Read more
Health: the gift of life
Health: more funding is needed for breastfeeding specialists
Every year in Ireland, approximately 350 people are diagnosed with multiple myeloma – a cancer of the plasma cells that are made in the bone marrow. Although it is a rare and incurable blood disorder, it is treatable and some patients can live a normal life.
To further explain, multiple myeloma is an abnormal protein produced in multiple sites (bones) in the body, causing bone damage and pain. Kidney damage also occurs because calcium is leaked from the damaged bones.
The most common symptoms, therefore, are persistent bone or back pain, as well as kidney problems, anaemia, recurring infections and fatigue.
However, the news related to this type of cancer is very positive, according to Mary Kelly, registered advanced nurse practitioner in haematology, based at the Midlands Regional Hospital, Tullamore. She has cared for myeloma patients for 25 years and is in no doubt about the progress in treatments.
“Patients with multiple myeloma are now living much longer as a result of the great treatments available,” she says. “Five-year patient survival rates have increased from 24% to over 70% so it’s very good news.”
Concern about patients back in 2006 led Mary to write a thesis on the lived experience of multiple myeloma patients. She found that isolation, lack of support and general lack of awareness of the illness were major concerns.
She subsequently set up the support charity, Multiple Myeloma Ireland in 2008, which is based in the Dóchas Centre in Tullamore. It is the first and longest-running support and information group for people living with the disease.
Groups across the country have now sprung up as a result and a podcast began during lockdown called Living with Myleoma which has been nominated for a Bullseye award in the Irish Podcast Awards.
Mary has three key messages for anyone who is newly diagnosed.

Advanced nurse practitioner in haematology Mary Kelly pictured with Mag.
“Firstly, this is a very treatable condition. Secondly, anyone with symptoms should get them checked out quickly and thirdly, there is a lot of support for anyone with this illness,” she says.
However, making a diagnosis can be challenging. “A lot of tests are needed and that’s one of the challenges for healthcare professionals in the community. GPs may only see one case during their career so they are not looking for it. It can often be a combination of vague symptoms; who isn’t tired, who doesn’t have back pain, or some bone pain? However, persistent, severe pain are indicators.
“Multiple myeloma can sometimes be missed, so if you’ve got recurring symptoms you should be advocating with your GP for further investigation.”
Mag Kirwan’s story
Mag and her husband, Ger, run Goatsbridge Trout Farm near Thomastown, Co Kilkenny. The 59-year-old developed a love of fitness training in 2015, but in late 2019 she got a bad pain in her shoulder.
“I went to my local physio first and then to a second physio as it wasn’t getting better,” explains Mag.
“Anti-inflammatories were suggested so I had to contact my GP to get a prescription. As it happened, a new doctor looked at blood tests that I had done a few months earlier. Noticing some unusual levels, he advised getting more tests done. After an MRI, he rang to say I had a mass (a tumour) in my shoulder.”
A bone specialist then diagnosed early multiple myeloma but after a bone biopsy and a PET scan, Mag was told that it was full-blown multiple myeloma.
“This meant a change in my treatment plan, eight months of chemotherapy and the harvesting of my own stem cells in order for me to develop new bone marrow.”
Mum-of-four Mag found her eldest son, Ned’s 21st birthday in February 2020 particularly difficult. “I kept wondering if I’d be around to see the next one turn 21, and so on,” she says.
If you’re lucky and you keep your body and head right, you can live long and well with this. That’s what I believe
However, once she had her treatment plan, she felt more positive. “I knew it would take a year or two of consolidation treatment after the stem cell transplant. During that time I worked when I could and isolated when I had to.”
Nearly three years on, Mag says practising gratitude helps her get on with life.
“I have a lot going for me. Fifteen years ago there were one or two drugs available – now several new ones have been approved so, even though it’s not curable, it’s treatable.
“If you’re lucky and you keep your body and head right, you can live long and well with this. That’s what I believe. I don’t think too far ahead, I trust my consultant and my trainer. I have a great family and I feel really blessed.”
Mag, one of 10 from the Goresbridge Horse Sales family, believes that she has learned resilience over her lifetime.
“My mother was 42 and two months away from having her 10th child when my father died. My brother Jack died later, aged 10, of measles. My mother continued to grow the family business to international success and reared and educated us all.
“Life teaches you resilience so then when something like this happens you’re able to fight it and get on with it. I really believe that the power of the mind is incredible and that exercise is great medicine.”
Dermot O’Leary’s story
When dad-of-five Dermot, a 65-year-old dairy farmer from Bandon, Co Cork, had a routine blood test in September 2015, it showed high protein levels in his blood. At first prostate issues were suspected but a few months later, in January 2016, multiple myeloma was diagnosed.
“I had no symptoms,” he says, “but looking back I’d often fall asleep at the table after supper. Maybe that was the start of it and I just didn’t recognise it.
“I was glad to have a diagnosis in a way but my doctor said ‘you do realise this is cancer?’ I didn’t I suppose, but it sank in over a couple of days.”
Dermot attended a support meeting in Tullamore in March 2016, ahead of starting treatment in April.
“I had a good chat with the people there,” he says, “and felt, after that, that I could handle what was happening. I was calving cows at the time and working away as normal. I wouldn’t be a worrier. I just got on with it.”
Looking back I’d often fall asleep at the table after supper. Maybe that was the start of it and I just didn’t recognise
He underwent a stem cell transplant, which involves tests to assess your general level of health, harvesting to collect the stem cells to be used in the transplant, conditioning ie treatment with chemotherapy and/or radiotherapy to prepare your body for the transplant. Then there is the transplantation of the stem cells and, after that, recovery.
“They take out stem cells (enough for two treatments if needed),” Dermot says, “then put them back in again following chemotherapy. There were a few tough days, but it wasn’t the end of the world either,” he says.
He has been on a maintenance drug called Revlimid since then and an aspirin every morning to avoid clots.
Dermot has been on the board of Multiple Myeloma Ireland since 2019 and set up a support group in Cork.
“Early diagnosis is vital,” he insists. “There are horror stories where sports people who have pain in their back just assume it’s the legacy of sport. The sooner you get myeloma diagnosed, the better. That’s why we’re trying to get the word out.
“Our support groups meet every second month. Being a member helps you feel that you’re not alone and you learn from others too.”
Multiple myeloma is a blood cancer that develops in plasma cells in the bone marrow – the soft, spongy tissue at the centre of your bones.
Myeloma affects multiple places in the body where bone marrow is normally active in an adult, ie within the bones.
Stem cell transplants for multiple myeloma sees a person’s own stem cells removed from the bone marrow and stored until needed. The cells given in a transplant can grow into healthy blood cells in the bone marrow.
Multiple Myeloma Ireland is now lobbying for funding for a database of patients living with the illness.
For more information, email info@multiplemyelomaireland.org or see multiplemyelomaireland.org or cancer.ie
Read more
Health: the gift of life
Health: more funding is needed for breastfeeding specialists









SHARING OPTIONS