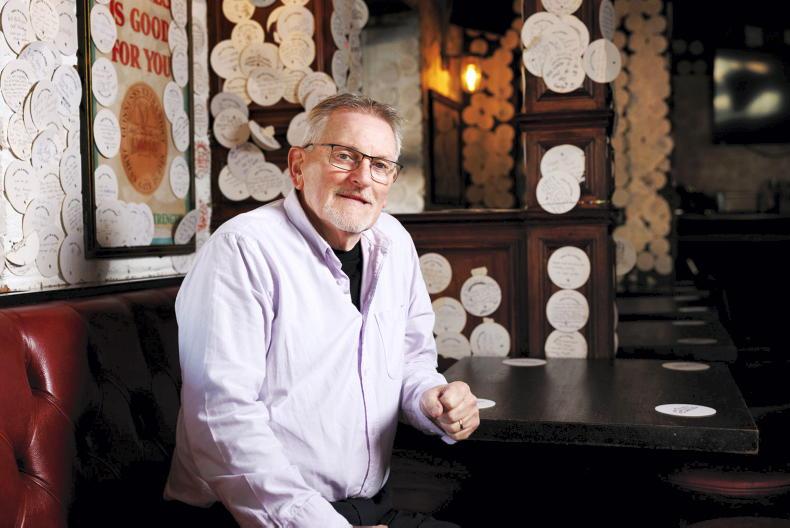
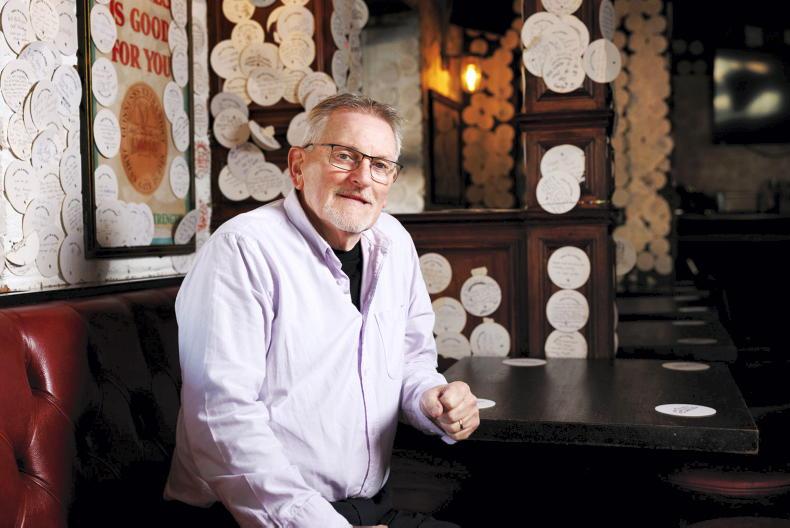
Men are generally uncomfortable talking about urinary and sexual function, but thanks to the efforts of one Donegal man, the conversation is beginning to happen.
Sixty-seven-year-old prostate cancer survivor, Gerry Connolly, says that talking about urinary incontinence (often a lasting side effect of prostate cancer) has been as difficult as discussing the cancer itself. Gerry, who lives just outside Stranorlar, was diagnosed with prostate cancer in 2013 and his prostate was removed about 18 months later.
Prostate cancer is the second most common cancer in men, after skin cancer. According to the National Cancer Registry Ireland, one in six men in Ireland will receive a prostate cancer diagnosis in their lifetime.
Fortunately, there are very high cure rates for men with early-stage prostate cancer. Dr Paul Hegarty, consultant urologic surgeon at the Mater Private Hospital in Cork and UPMC Whitfield Hospital Waterford, says: “Cure rates are around 90% following radical prostatectomy or radiotherapy.
“What we call ‘clinically significant cancers’ are offered radical therapy, which would be prostate removal or radiotherapy. That is generally for men who are thought to have a life expectancy of 10 years or more.”
Gerry was diagnosed “early on”, as his GP put him forward for Prostate Specific Antigen Testing (PSA). PSA is a product of the prostate gland, and raised levels suggest cancer or other prostate problems. “I was way over the threshold,” he says.
Following surgery to remove his prostate, Gerry’s recovery was “very good” but he describes “the shock” that later came with incontinence.
Side effects
According to Dr Hegarty, if men undergo radical prostatectomy, they have 10-20% chance of having incontinence in their first year after surgery.
“It is higher in the first few weeks after surgery (once the catheter has come out), but most improve in the subsequent weeks,” he says. “It can depend on the age of the man (over 70s are more likely to experience incontinence) and if the nerves running alongside the prostate are impacted in surgery.”
Gerry says he was told that incontinence “could be an issue” after prostate cancer, adding “the harsh reality came” when he was discharged from hospital and discovered “the whole side of the bed was soaking wet with urine” after his first night sleeping back at home.
“Incontinence is very, very frustrating. If you get up from a chair or sofa too quickly, you wet yourself. If you cough, you wet yourself, if you laugh, even if you stretch to get a cup down from the cupboard.
“It is a really psychological thing for a man to deal with – that you can’t control this unsightly feeling that you actually wet yourself.”
The side effects of prostate cancer can affect a person’s confidence, work and social life. “I used to make any excuse not to leave the house and I rarely left it for months,” says Gerry. He was afraid of leaking and smelling of urine, but also of not having a sanitary bin to dispose of a used pad.
Gerry has a constant supply of pads, wipes and incontinence pants wherever he goes. He jokingly refers to incontinence pants as “sumo wrestler pants”, adding “they’re another lovely experience to get used to.
“It’s bad enough having a wet pad, but when you have a wet sumo wrestler’s nappy that is a big, bulky thing, part of the reason you don’t go out is that you feel uncomfortable.”
Gerry did not disclose his issues with incontinence to his GP or even his family. “I think you’re still a bit unsure what’s happening to you,” he admits. “You’re getting over a cancer and you’re talking about the cancer – but you don’t talk about that part of it [incontinence].
When it comes to managing incontinence, Dr Hegarty recommends physiotherapy before and after surgery. He also mentions lifestyle modifications, like restricting caffeine intake.
In severe cases, there are also surgical procedures that men can undergo to manage incontinence, including the insertion of an artificial urinary sphincter or a synthetic mesh device or ‘sling’. This mesh device is made of the same material used in the mid-urethral sling to treat stress urinary incontinence; but the operation has been paused for women since 2018. “Women are being deprived of a good treatment, unfortunately,” says Dr Hegarty.

Paul Hegarty, consultant urologic surgeon at the Mater Private Hospital in Cork and UPMC Whitfield Hospital Waterford.
Erectile dysfunction
Erectile dysfunction is another side effect of prostate cancer, with some men reporting that it is the most difficult part of prostate cancer as they feel like they’re letting their partners down.
“When erectile dysfunction comes into your life, it can really change your intimacy. It is very important for couples, either prior to a man going for prostate surgery or immediately afterwards, to sit down and have that open discussion. My late wife Rose would have found that side of things difficult, telling me that she felt that I had lost interest in her. It’s difficult for the partners,” says Gerry.
“When you get the cancer diagnosis and you have a wife or a partner, the main focus is on dealing with the cancer. The incontinence and erectile dysfunction are things further down the line, but you don’t look at them seriously enough.”
Dr Hegarty explains that erectile dysfunction has “quite an effect on some men’s moods and satisfaction in life”.
“I have had the odd patient who says: ‘If I’d known it was going to be this bad, I wouldn’t have had my prostate out’.
“Communication is key,” he continues. “Learning to open up and talk about it is important and that takes a bit of practice. As well as erectile dysfunction, there can be orgasmic dysfunction and it will depend on if the nerves were spared or not in surgery.”
Dispose with Dignity
Gerry is one of the faces behind the ‘Dispose with Dignity’ campaign, an initiative backed by hygiene services company –
phs Group – with support from the Irish Cancer Society and the Irish Men’s Sheds Association.
The campaign, which launched at the start of November, aims to tackle the stigma of male incontinence, and improve access to hygiene facilities such as sanitary bins and vending products in men’s washrooms nationwide.
Of the 702 men surveyed for the research, more than half (52%) feel anxious about going out in public due to a lack of suitable toilet facilities. Over half (54%) have struggled to find a bin suitable for disposing of incontinence pads, with nearly half (46%) resorting to using disabled toilets or flushing products away (18%).
Gerry explains that access to sanitary bins in men’s cubicles would not only provide somewhere private to dispose of a pad, but also bring more visibility to prostate cancer.
“If there had been sanitary bins in men’s toilets, maybe I’d have felt I had options, somewhere private to change a pad and get on with my day,” he says. “If people see bins for men, it’ll start conversations and remind men to get tested early.
“But the main thing to remember is that early detection is key. And there is life after prostate cancer.”

Michelle Lonergan, cancer awareness nurse, Irish Cancer Society. \ Andres Poveda Photography.
The sooner prostate cancer is detected, the more successful the treatment outcomes.
Michelle Lonergan, cancer awareness nurse at Irish Cancer Society, says that symptoms related to prostate cancer are often urinary. “Symptoms can include getting up during the night more frequently to pass urine, trouble starting or stopping the flow of urine, any pain when passing urine or passing any blood in your urine.”
You can request a blood test called Prostate Specific Antigen (PSA) testing to screen for prostate cancer. From age of 50, men should ask their GP about prostate health. For men with family history of prostate cancer or black ethnicity, have that conversation from age 40.
The Irish Cancer Society has a support line operating Monday to Friday from 9am to 5pm, 1800 200 700, where you can speak to a cancer nurse. cancer.ie
Men are generally uncomfortable talking about urinary and sexual function, but thanks to the efforts of one Donegal man, the conversation is beginning to happen.
Sixty-seven-year-old prostate cancer survivor, Gerry Connolly, says that talking about urinary incontinence (often a lasting side effect of prostate cancer) has been as difficult as discussing the cancer itself. Gerry, who lives just outside Stranorlar, was diagnosed with prostate cancer in 2013 and his prostate was removed about 18 months later.
Prostate cancer is the second most common cancer in men, after skin cancer. According to the National Cancer Registry Ireland, one in six men in Ireland will receive a prostate cancer diagnosis in their lifetime.
Fortunately, there are very high cure rates for men with early-stage prostate cancer. Dr Paul Hegarty, consultant urologic surgeon at the Mater Private Hospital in Cork and UPMC Whitfield Hospital Waterford, says: “Cure rates are around 90% following radical prostatectomy or radiotherapy.
“What we call ‘clinically significant cancers’ are offered radical therapy, which would be prostate removal or radiotherapy. That is generally for men who are thought to have a life expectancy of 10 years or more.”
Gerry was diagnosed “early on”, as his GP put him forward for Prostate Specific Antigen Testing (PSA). PSA is a product of the prostate gland, and raised levels suggest cancer or other prostate problems. “I was way over the threshold,” he says.
Following surgery to remove his prostate, Gerry’s recovery was “very good” but he describes “the shock” that later came with incontinence.
Side effects
According to Dr Hegarty, if men undergo radical prostatectomy, they have 10-20% chance of having incontinence in their first year after surgery.
“It is higher in the first few weeks after surgery (once the catheter has come out), but most improve in the subsequent weeks,” he says. “It can depend on the age of the man (over 70s are more likely to experience incontinence) and if the nerves running alongside the prostate are impacted in surgery.”
Gerry says he was told that incontinence “could be an issue” after prostate cancer, adding “the harsh reality came” when he was discharged from hospital and discovered “the whole side of the bed was soaking wet with urine” after his first night sleeping back at home.
“Incontinence is very, very frustrating. If you get up from a chair or sofa too quickly, you wet yourself. If you cough, you wet yourself, if you laugh, even if you stretch to get a cup down from the cupboard.
“It is a really psychological thing for a man to deal with – that you can’t control this unsightly feeling that you actually wet yourself.”
The side effects of prostate cancer can affect a person’s confidence, work and social life. “I used to make any excuse not to leave the house and I rarely left it for months,” says Gerry. He was afraid of leaking and smelling of urine, but also of not having a sanitary bin to dispose of a used pad.
Gerry has a constant supply of pads, wipes and incontinence pants wherever he goes. He jokingly refers to incontinence pants as “sumo wrestler pants”, adding “they’re another lovely experience to get used to.
“It’s bad enough having a wet pad, but when you have a wet sumo wrestler’s nappy that is a big, bulky thing, part of the reason you don’t go out is that you feel uncomfortable.”
Gerry did not disclose his issues with incontinence to his GP or even his family. “I think you’re still a bit unsure what’s happening to you,” he admits. “You’re getting over a cancer and you’re talking about the cancer – but you don’t talk about that part of it [incontinence].
When it comes to managing incontinence, Dr Hegarty recommends physiotherapy before and after surgery. He also mentions lifestyle modifications, like restricting caffeine intake.
In severe cases, there are also surgical procedures that men can undergo to manage incontinence, including the insertion of an artificial urinary sphincter or a synthetic mesh device or ‘sling’. This mesh device is made of the same material used in the mid-urethral sling to treat stress urinary incontinence; but the operation has been paused for women since 2018. “Women are being deprived of a good treatment, unfortunately,” says Dr Hegarty.

Paul Hegarty, consultant urologic surgeon at the Mater Private Hospital in Cork and UPMC Whitfield Hospital Waterford.
Erectile dysfunction
Erectile dysfunction is another side effect of prostate cancer, with some men reporting that it is the most difficult part of prostate cancer as they feel like they’re letting their partners down.
“When erectile dysfunction comes into your life, it can really change your intimacy. It is very important for couples, either prior to a man going for prostate surgery or immediately afterwards, to sit down and have that open discussion. My late wife Rose would have found that side of things difficult, telling me that she felt that I had lost interest in her. It’s difficult for the partners,” says Gerry.
“When you get the cancer diagnosis and you have a wife or a partner, the main focus is on dealing with the cancer. The incontinence and erectile dysfunction are things further down the line, but you don’t look at them seriously enough.”
Dr Hegarty explains that erectile dysfunction has “quite an effect on some men’s moods and satisfaction in life”.
“I have had the odd patient who says: ‘If I’d known it was going to be this bad, I wouldn’t have had my prostate out’.
“Communication is key,” he continues. “Learning to open up and talk about it is important and that takes a bit of practice. As well as erectile dysfunction, there can be orgasmic dysfunction and it will depend on if the nerves were spared or not in surgery.”
Dispose with Dignity
Gerry is one of the faces behind the ‘Dispose with Dignity’ campaign, an initiative backed by hygiene services company –
phs Group – with support from the Irish Cancer Society and the Irish Men’s Sheds Association.
The campaign, which launched at the start of November, aims to tackle the stigma of male incontinence, and improve access to hygiene facilities such as sanitary bins and vending products in men’s washrooms nationwide.
Of the 702 men surveyed for the research, more than half (52%) feel anxious about going out in public due to a lack of suitable toilet facilities. Over half (54%) have struggled to find a bin suitable for disposing of incontinence pads, with nearly half (46%) resorting to using disabled toilets or flushing products away (18%).
Gerry explains that access to sanitary bins in men’s cubicles would not only provide somewhere private to dispose of a pad, but also bring more visibility to prostate cancer.
“If there had been sanitary bins in men’s toilets, maybe I’d have felt I had options, somewhere private to change a pad and get on with my day,” he says. “If people see bins for men, it’ll start conversations and remind men to get tested early.
“But the main thing to remember is that early detection is key. And there is life after prostate cancer.”

Michelle Lonergan, cancer awareness nurse, Irish Cancer Society. \ Andres Poveda Photography.
The sooner prostate cancer is detected, the more successful the treatment outcomes.
Michelle Lonergan, cancer awareness nurse at Irish Cancer Society, says that symptoms related to prostate cancer are often urinary. “Symptoms can include getting up during the night more frequently to pass urine, trouble starting or stopping the flow of urine, any pain when passing urine or passing any blood in your urine.”
You can request a blood test called Prostate Specific Antigen (PSA) testing to screen for prostate cancer. From age of 50, men should ask their GP about prostate health. For men with family history of prostate cancer or black ethnicity, have that conversation from age 40.
The Irish Cancer Society has a support line operating Monday to Friday from 9am to 5pm, 1800 200 700, where you can speak to a cancer nurse. cancer.ie








SHARING OPTIONS