what would you recommend for a farmer with back pain?
Last week, I outlined how to reduce risk factors around the farm in terms of tasks and the environment. Treatments for back pain should always start with non-surgical options. Most back pain is muscular and that is a good place to start.
Muscular pain happens because of both abnormal muscular patterns that develop but also because the muscle is attempting to compensate for the slow degenerative process that is occurring in the spinal column, you could call it “the spinal architecture”.
The National Institute for Clinical Excellence (NICE) in the UK Guidelines suggest exercise (not an issue for most farmers), manual therapies such as physiotherapy, physical therapy, chiropractic therapy and psychological therapies are effective.
I always mention the psychological component as we need to always be aware of the effects that chronic back pain can have on our mental health.
Over one fifth of adults in Ireland are overweight, so the spine has extra work to do in these cases. Therefore weight loss helps back pain.
And if these conservative measures fail?
Once a period of non-operative treatment has been tried and the pain is still there, it is worth looking into some form of imaging such as an MRI scan to further investigate the pain.
This scan will show up everything, including the “grey hair and wrinkles” that are evident in every spine as we get older, and they will usually show what is causing the back pain.
The leg or arm pain that accompanies these conditions usually settles down but can persist in some cases.
Spinal injections for the nerve root are usually effective for helping the pain to settle.
As most farmers are self-employed and without significant help, surgery for today’s farmer must allow them to recover quickly and get back to the job.
Spine surgery sounds risky, What do you say to your patients?
It is, I always use what is called the three-legged stool of consent – I tell my patients about the procedure, I type a letter summarising what we discuss and I email them an information booklet.
That way they can ask questions before deciding to proceed with surgery.
Over the last 10 years, I have noticed a big trend towards internet usage for information, particularly in our older patients, but we need to be careful about where we find that information and the quality of the website that provides it.
I work on the European Spine Society committee on the PatientLine group.
I often use this free online resource if patients want to look up their diagnosis and procedure.
What kind of operations do you
perform?
While I have trained on all spinal pathologies, including tumours, trauma, scoliosis etc, the operations that stand out for back pain are grouped into three options:
Decompression of a nerve root (back or neck pain that includes leg or arm pain).Fusion procedures (to stop painful movement often at an unstable or collapsed joint).Motion preservation procedures. After surgery, rehabilitation is very important to both help recovery and also to reduce the risk of further back pain.
Can you describe these in a little more detail?
Decompressions include a discectomy (the removal of herniated disc material), often in patients under 40 or a laminotomy (a procedure that removes part of the lamina of a vertebral arch).
The best international spinal research suggests that patients with over six weeks of pain from a slipped disc or three months in an older patient with spinal arthritis would benefit from surgery.
Discectomy or laminotomy can often be done as a keyhole procedure. The hospital stay can be as little as day-case surgery and a patient could be back to manual work within about six weeks.

On the left: an X-ray of the lumbar spine with decreased disc space between the vertebrae. On the right: after an ALIF procedure with an implant in the disc space.
Fusion procedures are technically more difficult, have more complications and take a longer time to recover from – more like six months.
Motion preservation procedures are in their infancy and do not suit most spinal patients. These ultimately resemble a form of disc replacement, usually in the lumbar or cervical spine.
Fusions remain the most common option for persistent spinal arthritis with painful joint instability. Sometimes patients may end up having a decompression and down the road, end up having a fusion also.
What? More surgery? Explain that please?
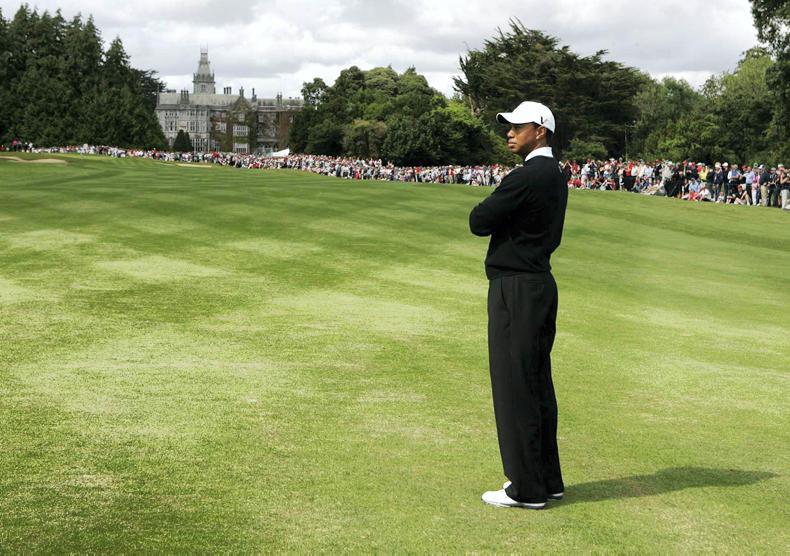
About 20% of adults who undergo spinal surgery end up having further spinal surgery at some point. I can give you Tiger Woods as an example.
He had horrendous back and leg pain which was, I assume from the high levels of spinal torque generated in hitting long drives.
He had two or three spinal decompressions before ultimately having a fusion procedure.
While he initially had success with a discectomy, his symptoms came back. As a young sports person, the surgeon wanted to initially avoid fusion surgery but he required it in the end. And then he won the Masters two years later.
Yes I heard about that. What did he have done?
Tiger had an anterior lumbar interbody fusion, or ALIF for short. What is different about this procedure is that the lumbar spine is approached from the front, through the belly.
At least in my experience, I find that my patients have less pain after the surgery as there is much less cutting of tissue, so they are ready to leave the hospital sooner.
They also have better spinal fusion than traditional procedures. The bone successfully knits together in 90% of cases, not 100%.
Beware though, most farmers want to get back to work too soon and any manual labour while this is healing will loosen the implant.
What is also really good about the ALIF is that the implant is a much closer fit to that of the original disc height than what can be achieved from more traditional spinal fusion operations through the back (of the back).

Consultant spine surgeon Derek Cawley.
Mr Derek Cawley is a spinal surgeon working in full-time private practice in Dublin. Further information on referral to his clinics are available on his website.
what would you recommend for a farmer with back pain?
Last week, I outlined how to reduce risk factors around the farm in terms of tasks and the environment. Treatments for back pain should always start with non-surgical options. Most back pain is muscular and that is a good place to start.
Muscular pain happens because of both abnormal muscular patterns that develop but also because the muscle is attempting to compensate for the slow degenerative process that is occurring in the spinal column, you could call it “the spinal architecture”.
The National Institute for Clinical Excellence (NICE) in the UK Guidelines suggest exercise (not an issue for most farmers), manual therapies such as physiotherapy, physical therapy, chiropractic therapy and psychological therapies are effective.
I always mention the psychological component as we need to always be aware of the effects that chronic back pain can have on our mental health.
Over one fifth of adults in Ireland are overweight, so the spine has extra work to do in these cases. Therefore weight loss helps back pain.
And if these conservative measures fail?
Once a period of non-operative treatment has been tried and the pain is still there, it is worth looking into some form of imaging such as an MRI scan to further investigate the pain.
This scan will show up everything, including the “grey hair and wrinkles” that are evident in every spine as we get older, and they will usually show what is causing the back pain.
The leg or arm pain that accompanies these conditions usually settles down but can persist in some cases.
Spinal injections for the nerve root are usually effective for helping the pain to settle.
As most farmers are self-employed and without significant help, surgery for today’s farmer must allow them to recover quickly and get back to the job.
Spine surgery sounds risky, What do you say to your patients?
It is, I always use what is called the three-legged stool of consent – I tell my patients about the procedure, I type a letter summarising what we discuss and I email them an information booklet.
That way they can ask questions before deciding to proceed with surgery.
Over the last 10 years, I have noticed a big trend towards internet usage for information, particularly in our older patients, but we need to be careful about where we find that information and the quality of the website that provides it.
I work on the European Spine Society committee on the PatientLine group.
I often use this free online resource if patients want to look up their diagnosis and procedure.
What kind of operations do you
perform?
While I have trained on all spinal pathologies, including tumours, trauma, scoliosis etc, the operations that stand out for back pain are grouped into three options:
Decompression of a nerve root (back or neck pain that includes leg or arm pain).Fusion procedures (to stop painful movement often at an unstable or collapsed joint).Motion preservation procedures. After surgery, rehabilitation is very important to both help recovery and also to reduce the risk of further back pain.
Can you describe these in a little more detail?
Decompressions include a discectomy (the removal of herniated disc material), often in patients under 40 or a laminotomy (a procedure that removes part of the lamina of a vertebral arch).
The best international spinal research suggests that patients with over six weeks of pain from a slipped disc or three months in an older patient with spinal arthritis would benefit from surgery.
Discectomy or laminotomy can often be done as a keyhole procedure. The hospital stay can be as little as day-case surgery and a patient could be back to manual work within about six weeks.

On the left: an X-ray of the lumbar spine with decreased disc space between the vertebrae. On the right: after an ALIF procedure with an implant in the disc space.
Fusion procedures are technically more difficult, have more complications and take a longer time to recover from – more like six months.
Motion preservation procedures are in their infancy and do not suit most spinal patients. These ultimately resemble a form of disc replacement, usually in the lumbar or cervical spine.
Fusions remain the most common option for persistent spinal arthritis with painful joint instability. Sometimes patients may end up having a decompression and down the road, end up having a fusion also.
What? More surgery? Explain that please?
About 20% of adults who undergo spinal surgery end up having further spinal surgery at some point. I can give you Tiger Woods as an example.
He had horrendous back and leg pain which was, I assume from the high levels of spinal torque generated in hitting long drives.
He had two or three spinal decompressions before ultimately having a fusion procedure.
While he initially had success with a discectomy, his symptoms came back. As a young sports person, the surgeon wanted to initially avoid fusion surgery but he required it in the end. And then he won the Masters two years later.
Yes I heard about that. What did he have done?
Tiger had an anterior lumbar interbody fusion, or ALIF for short. What is different about this procedure is that the lumbar spine is approached from the front, through the belly.
At least in my experience, I find that my patients have less pain after the surgery as there is much less cutting of tissue, so they are ready to leave the hospital sooner.
They also have better spinal fusion than traditional procedures. The bone successfully knits together in 90% of cases, not 100%.
Beware though, most farmers want to get back to work too soon and any manual labour while this is healing will loosen the implant.
What is also really good about the ALIF is that the implant is a much closer fit to that of the original disc height than what can be achieved from more traditional spinal fusion operations through the back (of the back).

Consultant spine surgeon Derek Cawley.
Mr Derek Cawley is a spinal surgeon working in full-time private practice in Dublin. Further information on referral to his clinics are available on his website.






SHARING OPTIONS