Prostate cancer is the most common cancer in males in Ireland so being aware of it and taking action if you have symptoms is very important.
Dr Richard Bambury, consultant medical oncologist at Cork University Hospital, stresses the importance of early diagnosis – and outlines the relevant symptoms.
“Any man who has new urinary symptoms - meaning that the flow of their urine has slowed down or that they are needing to go to the bathroom more frequently or they are needing to get up a lot at night - if they notice these symptoms, they should attend their GP for an assessment,” he says.
The good news is that these symptoms may not necessarily mean prostate cancer (it could be a less serious prostate issue) but they are symptoms that need to be evaluated, he states.
But what are the risk factors for prostate cancer?
“Advancing age is the main one and most of those diagnosed with it are in their late 60s,” says Dr Bambury who is based at Cork University Hospital (CUH).
Treatment
Treatment varies depending on the stage the cancer is discovered at and can range from surveillance, chemotherapy, radiotherapy, the newer brachytherapy and surgery in some cases.
“Some prostate cancers are very slow growing,” Dr Bambury says, “and unlikely ever to spread outside the prostate or cause any major health problems. Most cases of prostate cancers are picked up at an early stage and those cancers can be managed with what’s called surveillance. That’s where there’s a yearly check up with a urologist who makes sure there is no sign of the cancer progressing.”
About 1 in 10 are picked up when the cancer has spread, however.
“The other side of the coin is patients who have a prostate cancer that looks more aggressive and has more chance of spreading to the bones and other organs. It’s a life threatening condition if that happens.”
Non-surgical approaches
Surgery is not always necessary, however, and there are other approaches available for men who don’t want to have an operation or who might have other medical problems, which would mean that having an operation would be dangerous.
“All the options are discussed with the patient,” he says. “They can be treated with radiotherapy, which is essentially shooting high energy X-ray beams at the tumour. That’s a very good way to cure prostate cancer as well and it is as effective as surgery. Surgery and radiotherapy are the main options for localised prostate cancer.”
If the prostate cancer has spread there are ways to manage that as well. These approaches include hormonal therapy, where medication is used to put the cancer to sleep by decreasing the body’s testosterone level.
“We also have a number of newer hormonal and chemotherapy treatments available, which means that outcomes are much better, even for the worst type of prostate cancer.”
Brachytherapy is a newer type of treatment.
“This is a type of radiotherapy where the doctor inserts radioactive seeds directly into the prostate. That’s done instead of needing to fire radioactive beams from the outside. The advantage of this is that the brachytherapy has less effect on other organs because the seeds don’t affect the surrounding tissues. It is good for a localised cancer that hasn’t spread anywhere else but it’s not for everybody.”
New type of scan
Technological developments have meant that a new type of scan is also available in some hospitals - a PSNA PET scan. This is a diagnostic tool that uses a type of medical imaging called positron emission tomography (PET). PSMA stands for prostate specific membrane antigen, a protein found on the surface of prostate cancer cells.
“It can find tiny prostate cancer cells around the body that other scans can’t pick up. That gives us a better picture of where it has spread to. That extra information can direct our treatment approaches.”
Surgery- new developments
Thankfully there have been a lot of recent advances, he says, including robotic surgery, which can mean smaller incisions and earlier discharge from hospital.
“The cure rate is the same whether you do the operation by robotic surgery or conventional method but the complications or recovery times are quicker with the robotic approach. While it is not suitable for everybody it is a good option for some.”
PSA (prostate specific antigen) tests are often done as part of a male health GP check-up after the age of 50, but there are differing opinions in the medical world about whether regular PSA check-ups should be taken for all men or not, according to Dr Bambury.
If the prostate cancer has spread there are ways to manage that as well
“There are pros and cons to it. Each man, once they reach the age of 50, should talk to their GP about their individual circumstances as to whether routine PSA testing would be the right option for them or not. The important thing is to get any new urinary symptoms checked out”
He points out that there are rapid access prostate clinics set up in the HSE National Cancer Control Programme (NCCP) hospitals around the country where men can be directly referred by their GP.
“They can have an assessment with a urologist who can make a decision on what the best management is in conjunction with the patient, so I would urge people who have new symptoms to have them checked out.”
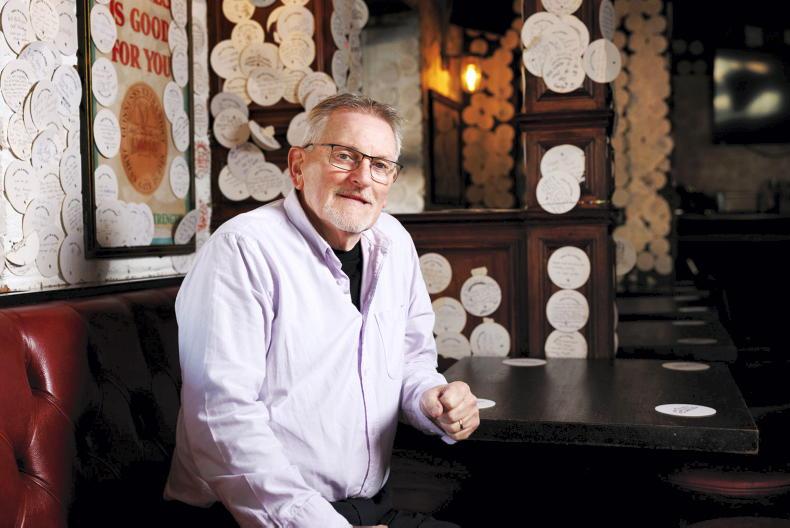
Mike Walsh, Lecturer in Agricultural Science in the South East Technology University (formerly WIT).
The message was ‘you kill this or it will kill you’
Mike had some tests in 2019 after GP concern about his PSA levels being unstable in annual “NCT” check-ups. Tests led to the discovery of a slight lump on one side of his prostate gland in May of that year. Biopsies followed.
Mike was at the Bloom Festival 2019 when his consultant rang him.
“There was a poor signal and lots of noise so I couldn’t hear what was being said initially,” he says, “but it turned out that I was being asked to go to the hospital as soon as possible.”
Next day he was given the news that he had early stage cancer and immediate treatment was advised.
“I asked the radiologist not to beat about the bush when giving me the news. The message was ‘you kill this or it will kill you’ and that treatment should start immediately. I talked to my wife Bernie about the treatment options and we decided to opt for hormonal treatment followed by brachytherapy followed by radiotherapy.”
The hormonal treatment started three days later on 6 June (tablets) and brachytherapy followed in September. As mentioned above, brachytherapy involved inserting radioactive pellets into the prostate gland (internal radiation).
Three years on Mike is doing well although his sleep is still disrupted.
“I’m not sure why that is but I don’t get more than three hours at a time. Overall though, I feel like I dodged a bullet. Some people in my age group haven’t been as lucky. That puts it in perspective.”
Mike’s message is “don’t wait if you have a concern” and “be sure to have your regular check ups”.
“You may not have any noticeable symptoms. I didn’t,” he says.
Benefits of exercise
Mike also emphasises the importance of exercise in recovery from cancer and how it helped him.
After putting on 10kg weight due to treatment and lack of exercise, he was determined to get fit again. Using a rowing machine and power walking, he slowly built up his strength and lost the gained weight.
“Exercise gets you out there and keeps your mind occupied too. Having a target to work to can help as well.”
Fundraiser challenge
Mike put his belief in exercise to the test in May 2021 when, along with friends in the Kilmacthomas Walking Club, he organised a Neverest hill climb (so called to tie in with his lack of sleep and record the Everest distance of 9000 feet in a different way).
He did it as a fundraiser for the Solas Cancer Support Centre in Waterford.
The challenge consisted of climbing Comeragh Mountain 34 times up and down (the equivalent of climbing Everest), climbing 275m each time over a distance of 1 km.
“The trial was continuous - 35 hours and we needed a long day, a full moon and fine weather,” he says. “That’s why we decided to go for the end of May. It was also the second anniversary of my diagnosis.”
Mike says that he wanted to do the challenge because it was comparable to his cancer recovery experience.
“You start at the bottom and you know it’s going to be an uphill trek and you might think you are never going to get to the end of this, but with every step you’re getting a little bit further. The reality is, of course, that everyone doesn’t make it to the top but you give it your best shot. That’s what we were looking at with the challenge we set up. It wasn’t easy but we finished with six minutes of the allotted 35 hours to spare.”
Mike is now planning a hill climb for the Irish Cancer Society.
Read more
Protect your children: store medicines and pesticides safely
Health: why we need to be more aware of kidney disease
Prostate cancer is the most common cancer in males in Ireland so being aware of it and taking action if you have symptoms is very important.
Dr Richard Bambury, consultant medical oncologist at Cork University Hospital, stresses the importance of early diagnosis – and outlines the relevant symptoms.
“Any man who has new urinary symptoms - meaning that the flow of their urine has slowed down or that they are needing to go to the bathroom more frequently or they are needing to get up a lot at night - if they notice these symptoms, they should attend their GP for an assessment,” he says.
The good news is that these symptoms may not necessarily mean prostate cancer (it could be a less serious prostate issue) but they are symptoms that need to be evaluated, he states.
But what are the risk factors for prostate cancer?
“Advancing age is the main one and most of those diagnosed with it are in their late 60s,” says Dr Bambury who is based at Cork University Hospital (CUH).
Treatment
Treatment varies depending on the stage the cancer is discovered at and can range from surveillance, chemotherapy, radiotherapy, the newer brachytherapy and surgery in some cases.
“Some prostate cancers are very slow growing,” Dr Bambury says, “and unlikely ever to spread outside the prostate or cause any major health problems. Most cases of prostate cancers are picked up at an early stage and those cancers can be managed with what’s called surveillance. That’s where there’s a yearly check up with a urologist who makes sure there is no sign of the cancer progressing.”
About 1 in 10 are picked up when the cancer has spread, however.
“The other side of the coin is patients who have a prostate cancer that looks more aggressive and has more chance of spreading to the bones and other organs. It’s a life threatening condition if that happens.”
Non-surgical approaches
Surgery is not always necessary, however, and there are other approaches available for men who don’t want to have an operation or who might have other medical problems, which would mean that having an operation would be dangerous.
“All the options are discussed with the patient,” he says. “They can be treated with radiotherapy, which is essentially shooting high energy X-ray beams at the tumour. That’s a very good way to cure prostate cancer as well and it is as effective as surgery. Surgery and radiotherapy are the main options for localised prostate cancer.”
If the prostate cancer has spread there are ways to manage that as well. These approaches include hormonal therapy, where medication is used to put the cancer to sleep by decreasing the body’s testosterone level.
“We also have a number of newer hormonal and chemotherapy treatments available, which means that outcomes are much better, even for the worst type of prostate cancer.”
Brachytherapy is a newer type of treatment.
“This is a type of radiotherapy where the doctor inserts radioactive seeds directly into the prostate. That’s done instead of needing to fire radioactive beams from the outside. The advantage of this is that the brachytherapy has less effect on other organs because the seeds don’t affect the surrounding tissues. It is good for a localised cancer that hasn’t spread anywhere else but it’s not for everybody.”
New type of scan
Technological developments have meant that a new type of scan is also available in some hospitals - a PSNA PET scan. This is a diagnostic tool that uses a type of medical imaging called positron emission tomography (PET). PSMA stands for prostate specific membrane antigen, a protein found on the surface of prostate cancer cells.
“It can find tiny prostate cancer cells around the body that other scans can’t pick up. That gives us a better picture of where it has spread to. That extra information can direct our treatment approaches.”
Surgery- new developments
Thankfully there have been a lot of recent advances, he says, including robotic surgery, which can mean smaller incisions and earlier discharge from hospital.
“The cure rate is the same whether you do the operation by robotic surgery or conventional method but the complications or recovery times are quicker with the robotic approach. While it is not suitable for everybody it is a good option for some.”
PSA (prostate specific antigen) tests are often done as part of a male health GP check-up after the age of 50, but there are differing opinions in the medical world about whether regular PSA check-ups should be taken for all men or not, according to Dr Bambury.
If the prostate cancer has spread there are ways to manage that as well
“There are pros and cons to it. Each man, once they reach the age of 50, should talk to their GP about their individual circumstances as to whether routine PSA testing would be the right option for them or not. The important thing is to get any new urinary symptoms checked out”
He points out that there are rapid access prostate clinics set up in the HSE National Cancer Control Programme (NCCP) hospitals around the country where men can be directly referred by their GP.
“They can have an assessment with a urologist who can make a decision on what the best management is in conjunction with the patient, so I would urge people who have new symptoms to have them checked out.”
Mike Walsh, Lecturer in Agricultural Science in the South East Technology University (formerly WIT).
The message was ‘you kill this or it will kill you’
Mike had some tests in 2019 after GP concern about his PSA levels being unstable in annual “NCT” check-ups. Tests led to the discovery of a slight lump on one side of his prostate gland in May of that year. Biopsies followed.
Mike was at the Bloom Festival 2019 when his consultant rang him.
“There was a poor signal and lots of noise so I couldn’t hear what was being said initially,” he says, “but it turned out that I was being asked to go to the hospital as soon as possible.”
Next day he was given the news that he had early stage cancer and immediate treatment was advised.
“I asked the radiologist not to beat about the bush when giving me the news. The message was ‘you kill this or it will kill you’ and that treatment should start immediately. I talked to my wife Bernie about the treatment options and we decided to opt for hormonal treatment followed by brachytherapy followed by radiotherapy.”
The hormonal treatment started three days later on 6 June (tablets) and brachytherapy followed in September. As mentioned above, brachytherapy involved inserting radioactive pellets into the prostate gland (internal radiation).
Three years on Mike is doing well although his sleep is still disrupted.
“I’m not sure why that is but I don’t get more than three hours at a time. Overall though, I feel like I dodged a bullet. Some people in my age group haven’t been as lucky. That puts it in perspective.”
Mike’s message is “don’t wait if you have a concern” and “be sure to have your regular check ups”.
“You may not have any noticeable symptoms. I didn’t,” he says.
Benefits of exercise
Mike also emphasises the importance of exercise in recovery from cancer and how it helped him.
After putting on 10kg weight due to treatment and lack of exercise, he was determined to get fit again. Using a rowing machine and power walking, he slowly built up his strength and lost the gained weight.
“Exercise gets you out there and keeps your mind occupied too. Having a target to work to can help as well.”
Fundraiser challenge
Mike put his belief in exercise to the test in May 2021 when, along with friends in the Kilmacthomas Walking Club, he organised a Neverest hill climb (so called to tie in with his lack of sleep and record the Everest distance of 9000 feet in a different way).
He did it as a fundraiser for the Solas Cancer Support Centre in Waterford.
The challenge consisted of climbing Comeragh Mountain 34 times up and down (the equivalent of climbing Everest), climbing 275m each time over a distance of 1 km.
“The trial was continuous - 35 hours and we needed a long day, a full moon and fine weather,” he says. “That’s why we decided to go for the end of May. It was also the second anniversary of my diagnosis.”
Mike says that he wanted to do the challenge because it was comparable to his cancer recovery experience.
“You start at the bottom and you know it’s going to be an uphill trek and you might think you are never going to get to the end of this, but with every step you’re getting a little bit further. The reality is, of course, that everyone doesn’t make it to the top but you give it your best shot. That’s what we were looking at with the challenge we set up. It wasn’t easy but we finished with six minutes of the allotted 35 hours to spare.”
Mike is now planning a hill climb for the Irish Cancer Society.
Read more
Protect your children: store medicines and pesticides safely
Health: why we need to be more aware of kidney disease








SHARING OPTIONS